Antibiotic advantage in decline
 The Australian Commission on Safety and Quality in Healthcare (ACSQHC) says rampant over-prescription is adding to the ‘superbug’ threat.
The Australian Commission on Safety and Quality in Healthcare (ACSQHC) says rampant over-prescription is adding to the ‘superbug’ threat.
The ACSQHC has issued a new report on antibiotic prescription in Australia, in which it argues that about 23 per cent of antibiotic prescriptions in hospitals are ‘inappropriate’.
“More than 50 per cent of people with colds and other upper respiratory tract infections were prescribed antimicrobials when not recommended by guidelines,” said Professor John Turnidge, ACSQHC senior medical advisor.
He said the vast majority of infections in the community are viral, not bacterial, and so they do not require any antibiotics.
“It's a big problem. We have to convince both the GP and the patient that an antibiotic is not required.”
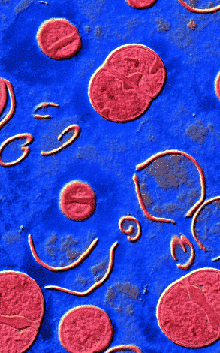
The World Health Organisation has called antimicrobial resistance an “increasingly serious threat to global public health”, with the massive over-use of the drugs allowing bacteria to rapidly evolve protections against their effects.
The new report looks at the emergence of modern superbugs, raising concerns about e-coli and VRE (vancomycin resistant organisms) in particular.
Professor Turnidge says there is an odd effect at play in Australian hospitals that leads to about a third of patients getting unnecessary antimicrobial treatments.
But because certain antibiotics are either not on to the Pharmaceutical Benefits Scheme, or only on very restricted use, rates of resistances to some bacteria were high and others very low.
He calls it “the Australian paradox”.
There are efforts to reverse the trend in hospitals, with rates of resistant golden staph (MRSA) dropping after initiatives like hand hygiene programs.
“Rates of MRSA is rising in the community and we think high use of antibiotics in the community is contributing,” Professor Turnidge said.
More must be done, the experts say, as Australia faces a future without viable therapeutic options for serious infections if its current over-use continues.








 Print
Print