Experts propose healthy shift
 Australia’s health system is criticised for failing both users and providers, but change is possible, according to experts.
Australia’s health system is criticised for failing both users and providers, but change is possible, according to experts.
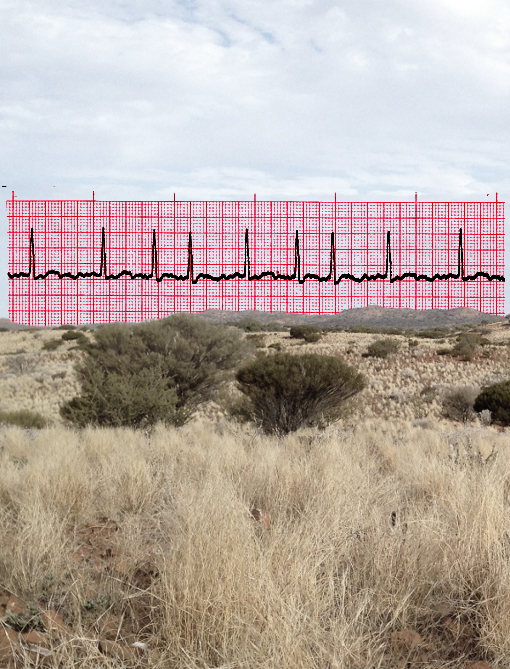
The University of Queensland’s Professor Claire Jackson and Professor Diana O’Halloran from Western Sydney University sya there are increasing signs that “our strained health care system is pushing the stress performance curve into the red”.
“Benchmarks of hospital activity demonstrate ongoing difficulty; Local Hospital Networks scramble to meet demand despite annual federal government funding increases of 6.5 per cent; and the grey literature attests to the unfolding human impact behind the figures,” they said.
“Patients deteriorate waiting for specialist assessment, and junior doctors find themselves trapped in increasingly overstretched, dysfunctional work environments.”
Despite royal commissions and inquiries into aged care, mental health, productivity and system change, they found little concrete change had been forthcoming.
“Put simply, our health system is fragmented, inefficient, inflexible, and organisation- rather than person-focused; locked into decline without significant structural, governance and funding reform,” they said.
“State governments continue to fund acute and specialised service delivery along historical activity-based lines, with the Commonwealth taking the heavy lifting on community general practice, pathology, radiology, specialist and aged care services.
“Without governance alignment, this allows little opportunity to develop fully integrated models of care.”
Professors Jackson and O’Halloran say the situation in New South Wales provides some hope and a way forward.
“New South Wales has arguably been the most consistent [of the states], exploring integrated care over 15 years from early HealthOne demonstration sites to current maturing co-commissioning models,” the said.
In Western Sydney, for example, successful Integrated Care initiatives have been progressively incorporated into co-commissioning models of care.
This approach has been used to create specialist rapid access clinics for patient stabilisation and general practitioner support, which have led to a 32 per cent reduction in emergency department presentations and a 34 per cent reduction in admissions
Efforts have also led to diabetes outreach in general practice being offered via specialist case conferencing, enhancing general practice team capability and patient clinical outcomes.
Also, non-prescribing pharmacists in general practices have been able to provide measurable change or deprescribing in complex care patients.
Professors Jackson and O’Halloran said the NSW experience shows that “despite the many barriers to change, they have succeeded in delivering effective new models of care”.
“Courage and leadership are needed to turn our struggling health system around,” they concluded.
“We must build new regional governance structures that bring the critical organisations and service providers together, enabling joint planning, pooled funding and the codesign, delivery, and continuing evaluation of relevant new health initiatives.
“We must recognise that an increasing number of Australians need care that is complex and requires coordination by their ongoing community team in partnership with the broader health and social care sector — not care in siloes.”








 Print
Print